Iron deficiency is one of the most common causes of anemia, and results in a microcytic anemia with an elevated RDW and inadequate reticulocytosis. Iron is ubiquitous in the American diet. Deficiency may result from menstrual blood loss in female patients, but when iron deficiency is present in adult males and postmenopausal females, an underlying pathologic process of the gastrointestinal tract, particularly malabsorption, malignancies, or other sources of hemorrhaging, must be suspected. Inadequate iron stores results in decreased hemoglobin synthesis, also the membranes of red cells in iron deficient patients are stiff and this results in premature splenic destruction.
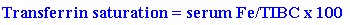
Laboratory abnormalities in iron deficiency anemia include a microcytic, hypochromic anemia with an elevated RDW. A reactive thrombocytosis may be noted but is not essential for diagnosis. In fact, one-third of patients have an associated thrombocytopenia noted on their CBC. Serum ferritin, iron, and iron saturation are all depressed although the serum total iron binding capacity (TIBC) is characteristically increased. Also, the calculated value for the transferrin saturation, as follows,
is characteristically depressed (usually less than 15%). When the serum ferritin is depressed, the diagnosis can be firmly established. The problem arises when the ferritin is in the normal range or elevated because this does not exclude the diagnosis. The serum ferritin may be falsely elevated in patients who also have hepatic cirrhosis, Hodgkins disease, acute leukemias, solid tumors, fever, inflammation, and chronic renal failure. If the diagnosis remains in doubt, then testing for serum transferrin receptor level or red blood cell protoporphrin level may establish the diagnosis. In cases of iron deficiency, the serum transferin receptor level and the red blood cell protoporphrin level increase. If the diagnosis is still in doubt, examination of bone marrow stores for iron by staining with Prussian blue reveals an absence of iron deposits in macrophages thus establishing the diagnosis.
Physical signs associated with iron deficiency include koilonychia (spoon-shaped nails) or more commonly, dry, brittle, ridged nails. Occasionally, patients may complain of a sore tongue, or physical examination may reveal atrophy of the lingual papillae and angular stomatitis (erosions at the corners of the mouth). Plummer-Vinson syndrome is characterized by iron deficiency anemia and esophageal webs. Patients afflicted with Plummer-Vinson syndrome usually require esophageal dilatation when dysphagia occurs and they may later develop esophageal carcinoma. Patients with iron deficiency may also complain of pica, a hunger for ice, clay, cornstarch, or other unusual substances.
Once iron deficiency is diagnosed in males and postmenopausal females, a complete workup for gastrointestinal pathology must be undertaken (the same workup should also be done in any female patient whose iron deficiency cannot be attributed to menstrual bleeding). Iron deficiency may also be secondary to malabsorption in such conditions as celiac disease, inflammatory bowel disease, or post gastric bypass. Infestation with hookworm may lead to iron deficiency; therefore, stool samples to screen for ova and parasites should be sent in appropriate cases. Patients on hemodialysis often manifest iron deficiency as a contributing cause of their anemia. Hemodialysis patients are prone to iron deficiency anemia secondary to the chronic blood loss that occurs during hemodialysis and should receive iron therapy to maintain a ferritin above 100 and a transferrin saturation above 20.
Therapy for iron deficiency consists of oral iron supplementation. This is usually accomplished with FeSO4 300 mg PO QD which is then incrementally increased over three weeks to FeSO4 300 mg PO TID. Oral iron should be initiated slowly to help prevent gastrointestinal irritation, which includes cramping, constipation or diarrhea (as these decrease compliance). Physicians often begin treatment with empiric stool softener therapy. Iron should be given 1 hour before meals as absorption is decreased when administered with food. In refractory cases, ascorbic acid (vitamin C) may be added to increase iron absorption. If gastrointestinal side effects are intolerable, iron may be administered with meals, the dose may be decreased or administered via pediatric liquid preparations. Once iron therapy has been initiated, the response to therapy may be gauged by comparing the baseline and follow-up values of the reticulocyte count, ferritin, and hemoglobin/hematocrit. The maximal reticulocytosis usually occurs after 7 to 10 days of therapy. The hemoglobin/hematocrit begins to improve after 2 to 3 weeks of therapy but usually requires approximately 2 months of therapy to normalize. Once the hemoglobin/hematocrit returns to normal, measurement of the serum ferritin serves as an effective way to assure that iron stores have been replenished and that iron therapy may be discontinued unless the underlying lesion remains uncorrected. Cases refractory to oral therapy do occur. In this instance, parenteral iron (for either intravenous or intramuscular administration) is available.